Long-Term Testosterone Therapy Improves Cardiometabolic Function and Reduces Risk of Cardiovascular Disease: Real-Life Results

Most men with testosterone deficiency need testosterone therapy for the rest of their life in order to achieve and maintain best possible health outcomes. Therefore, studies that investigate the effects of testosterone therapy in real-life are needed, to shed light on adherence and health outcomes in routine clinical practice.[1] While randomized controlled trials (RCTs) are gold standard in medical research [2, 3], RCTs are conducted in highly controlled environments and therefore their results may not carry over to the uncontrolled setting of real-life.[1] It is increasingly recognized that conclusions drawn from RCTs are not always a useful aid for decision-making because evaluating the value of a drug or technology requires an understanding of its impact on current clinical practice and management of patients in a real-life setting.[4]
A series of “real-life studies” have been conducted, all showing numerous health benefits of testosterone therapy in testosterone deficient (hypogonadal) men and confirming its safety, with an observation period of up to 17 years.[5-23] Here I summarize the results from the most recent real-life study, published February 9th 2017 in the Journal of Cardiovascular Pharmacology and Therapeutics which investigated the long-term effects and safety of testosterone therapy for up to 8 years in testosterone deficient men attending a urological office.[5] Differences in cardiovascular risk factors and deaths with testosterone therapy were compared to those seen in testosterone deficient men not receiving testosterone therapy but attending the same urological office.[5]
Key Points
- Long-term testosterone therapy for 8 years in obese men with testosterone deficiency reduces deaths and non-fatal heart attacks and strokes, compared to men not receiving testosterone therapy.
- The testosterone-group has an estimated reduction in deaths (mortality) between 66% and 92% compared to non-treated men.
- As expected, hemoglobin and hematocrit increased in the testosterone treated group, but levels remained within the physiological reference ranges.
- In the testosterone treated group, 7 patients (1.9%) were diagnosed with low-grade prostate cancer. In the untreated (control) group 12 patients (4.1%) were diagnosed with prostate cancer.
- This study confirmed the well documented improvements in lipid profile, especially reduction in non-HDL levels, and glycemic control (marked reduction in HbA1c from diabetic to normal glycemia).
- Being conducted in a real-life setting – as opposed to a controlled study environment – this study provides evidence that long-term testosterone therapy is both effective, safe and feasible in clinical practice, and importantly results in a reduction in "hard clinical endpoints".
What is known
Numerous studies have shown that testosterone therapy reduces waist circumference, body fat mass, blood pressure, blood glucose and HbA1c, increases lean body mass and insulin sensitivity, and improves lipid profiles.[9, 15, 24-30] Since obesity, dyslipidemia, insulin resistance, hyperglycemia, metabolic syndrome, hypertension and diabetes are well established cardiovascular risk factors, any therapeutic modality that ameliorates these components is expected to reduce cardiovascular risk. Despite this, a few flawed studies alleged that testosterone therapy would increase cardiovascular risk.[31-34] However, after having reviewed the available evidence on testosterone therapy and cardiovascular risk [35], the FDA denied the petition to place a black box warning about cardiovascular risk on testosterone products [36] and the European Medicines Agency (EMA) denied the allegations that testosterone therapy would increase cardiovascular risk.[37] Below are the results from a new long-term study which confirms the safety of testosterone therapy and actually shows reduced cardiovascular risk and mortality.[5]
What this study adds
Of 656 men (mean age: 61 years) with total testosterone levels 12.1 nmol/L (349 ng/dL) or lower and symptoms of hypogonadism, 360 received testosterone undecanoate injections 1000 mg every 12 weeks following an initial 6-week interval, for up to 10 years. This treatment group was compared to a control group made up of 296 men who had opted to not receive testosterone therapy. Measurements were taken at least twice a year and 8-year data were analyzed for the outcomes summarized in table 1.
Table 1: Effect of long-term (8 years) testosterone therapy on testosterone levels and metabolic outcomes.[5]
Note: All changes are significant unless stated otherwise.
Safety Parameters
As expected, hemoglobin and hematocrit increased in the testosterone treated group, but levels remained within the physiological reference ranges.
In the testosterone treated group 7 patients (1.9%) were diagnosed with low-grade prostate cancer. In the untreated (control) group 12 patients (4.1%) were diagnosed with prostate cancer.
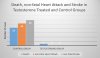
Death (mortality), nonfatal heart attack and stroke
There were 26 nonfatal heart attacks and 30 nonfatal strokes in the control group and none in the testosterone-treated group. There were 2 deaths in the testosterone-treated group, none was related to cardiovascular events. One was attributed to postsurgical thromboembolism and the other due to traffic accident. In the non-treated control group, there were 21 deaths, 19 of which were due to cardiovascular events (5 heart attacks, 4 stroke, 7 heart failure, 2 thromboembolism, 1 lung embolism).
The estimated reduction in mortality for the testosterone-group was between 66% and 92%. Figure 1 illustrates the differences in mortality, heart attack and stroke incidences between the groups.
Figure 1: Differences in mortality, heart attack and stroke between testosterone treated men and non-treated men.

Comments
This is the first long-term observational study that includes a comparison (control) group.[5] It confirms the safety and efficacy found in previous long-term real-life studies [5-23] and adds new important data. Several findings in this study deserve attention.
Liver function enzymes
The marked reduction in liver function enzymes in the testosterone treated group may suggest a potential reduction in liver fat content and inflammatory activity.[38, 39] It has previously been demonstrated that testosterone therapy reduces liver fat (accurately measured by CT imaging) in obese men.[40] There is a significant correlation between abdominal obesity and liver fat content (determined by liver biopsy during obesity surgery in severely obese men) [41] and numerous epidemiological studies shown that lower testosterone levels are associated with the development of NAFLD.[42] Considering that the prevalence of nonalcoholic fatty liver disease (NAFLD) is especially high in obese men [43], this merits further investigation.
Glycemic control
HbA1c is used to diagnose prediabetes and diabetes. The threshold for diabetes is HbA1c ≥ 6.5% and prediabetes is present when HbA1c is between 5.7% and 6.49%.[44, 45] As seen in table 1, testosterone treatment reduced glycemia from the diabetic range (HbA1c 6.9%) to normal range (HbA1c 5.6%). Going from diabetic glycemia to normal glycemia is a marked improvement, as most interventions only reduce glycemia from prediabetic to normal or diabetic to prediabetic. As expected, in the control group there was a worsening in glycemic control with an increase in HbA1c from 6.1% to 6.4%, to near diabetic glycemia (HbA1c 6.5%).
Pulse pressure
Pulse pressure (calculated as systolic blood pressure – diastolic blood pressure) is a marker of arterial stiffness [46-48] and is associated with greater risk of cardiovascular and all-cause mortality.[49] This study found a significant reduction in pulse-pressure in the testosterone treated group by 5 mmHg, while no change was seen in the control group. The importance of pulse pressure was highlighted in a study which found that a high pulse pressure in men is an independent predictor of cardiovascular mortality in both hypertensives and in those considered as having normal blood pressure, and it was suggested that this parameter can be useful when evaluating cardiovascular risk.[50]
Rate-pressure product
The rate-pressure product (RPP) (calculated as the product of heart rate and systolic blood pressure) is a reliable indicator of myocardial oxygen consumption and hemodynamic stress, and it is widely used clinically, especially in exercise interventions and rehabilitation.[51, 52] The rate pressure product (RPP) is associated with myocardial perfusion imaging (MPI) and it has been suggested that the cardiovascular risk with (pre)hypertension may be linked to the rate pressure product and BMI.[53] The study reported here found a significant reduction in RPP and significant increase in RPP in the testosterone and control groups, respectively.[5] This suggests that testosterone therapy may improve cardiac oxygen efficiency and reduce hemodynamic stress.
non-HDL cholesterol
This study is also notable for reporting a marked reduction in non-HDL cholesterol (non-HDL or non-HDL-C).[5] When triglyceride levels exceeds 150 mg/dL – as is commonly seen in patients with the metabolic syndrome, obesity, diabetes and cardiovascular disease - LDL particle number, apoB and VLDL levels increase without concomitant elevations in LDL-C.[54-56] Thus, non-HDL is more reflective of atherogenicity in people with elevated triglycerides.[57]
Several society guidelines for management of dyslipidemia for cardiovascular disease have recently added non-HDL as a primary treatment target. The International Atherosclerosis Society (IAS) Position Paper on the management of dyslipidemia considers non-HDL as an alternative to LDL-C as target of therapy, and actually favors adoption of non-HDL as the major target of lipid-lowering therapy.[57] The IAS expects that in future guidelines non-HDL will replace LDL-C as the best treatment target.
The European Society of Cardiology (ESC) / European Atherosclerosis Society (EAS) guideline states that non-HDL can provide a better risk estimation compared with LDL-C, in particular in patients with the metabolic syndrome or diabetes, who commonly have elevated triglyceride levels.[58]
Notably, the National Lipid Association (NLA) states that while non-HDL and LDL-C are co-primary treatment targets, non-HDL is the superior treatment target for modification.[59] Non-HDL levels and changes during treatment of dyslipidemia are more strongly associated with reduced risk for atherosclerotic coronary heart disease (CHD) than changes in LDL-C, or on-treatment levels of LDL-C.[59]
According to the 2017 AACE, ACE Dyslipidemia Clinical Practice Guidelines Update, the non-HDL treatment goal is 130 mg/dL for patients with two other risk factors, and 100 mg/dL for patients with two other risk factors plus diabetes or coronary, carotid or peripheral vascular disease.[60] In light of this, the marked reduction in non-HDL from 224 mg/dL to 113 mg/dL in testosterone treated men (and increase from 194 mg/dL to 201 mg/dL in non-treated men) should be highlighted.
Cardiovascular events and deaths
Regarding the debated issue of testosterone therapy and major cardiovascular events and mortality it is of particular interest is that there were only 2 deaths in the testosterone treated group, and none was related to cardiovascular events. Notably, in the non-treated control group there were 21 deaths, 19 of which were related to cardiovascular events. Furthermore, there were 26 nonfatal heart attacks and 30 nonfatal strokes in the control group but none in the T-treated group. In addition to all the beneficial changes in waist circumference reduction, weight loss and metabolic parameters that many studies have shown before, this is the first long-term study with a control (non-testosterone treated) group showing that this actually translates into reductions “hard clinical outcomes” in real-life.
The reduced incidence of heart attack, stroke, and death in testosterone treated hypogonadal men is in agreement with prior observational studies [12, 61-71] and two large meta-analyses of RCTs.[72, 73] The safety and cardiovascular protection of testosterone therapy was confirmed in the Testosterone Trials RCT, which found that during the follow-up year after the first year of testosterone therapy, there were 8 heart attacks in the placebo group compared to 1 in the testosterone group.[74] The longest duration RCT conducted at this point lasted for 3 years and also confirmed the safety of testosterone therapy.[75] An interesting finding in this study – which was not reported in the abstract - was that in men not taking statins, one marker of atherosclerosis (coronary artery calcium) was significantly lower in the testosterone group than in the placebo group.[75]
It is also notable that a another real-life study of men with testosterone deficiency and a history of cardiovascular disease, who received testosterone therapy for up to 8 years, no patient suffered a major adverse cardiovascular event during the full observation time.[12] In this study, cardio-metabolic parameters (lipid profile, glycemic control, blood pressure, heart rate, and pulse pressure), weight and waist circumference all improved significantly and sustainably [12], similarly to the results found in the study reported here.[5] Importantly, these improvements occurred even though patients were treated with statins, which suggests that statin treatment alone is inadequate. Thus, testosterone therapy may also be effective as an add-on treatment for secondary prevention of cardiovascular events in testosterone deficient men with a history of cardiovascular disease.[12]
Clinical practice relevance
Achievement of therapeutic testosterone levels - i.e. testosterone levels high enough (within the physiological range) – is essential for health benefits to occur.[66] The study reported here provides critical information on the long-term safety and effectiveness of testosterone therapy in clinical practice, as well as especially relevant data on adherence in the general population of men attending urological clinics.[5] It is notable that patients in the testosterone treated group achieved 100% medication adherence, as the testosterone injections were given in the doctor’s office and documented. This shows that injections of testosterone undecanoate at 12-week intervals is practically feasible in routine clinical practice, even in the long-term (the maximal observation duration was 10 years).[5]
The combined evidence base from both RCTs [72, 73] and observational studies [12, 61-70] is now strongly supportive of beneficial cardiovascular effects of testosterone therapy in hypogonadal men, which is accompanied by a reduction in cardiovascular mortality. In obese men, long-term testosterone therapy with testosterone undecanoate injections at 12 week intervals is clearly feasible in routine clinical practice and results in sustained weight loss and reductions in waist circumference and BMI without weight regain.[5-23] Interestingly, the 8 year weight loss of 17-24% with testosterone therapy [5] compares favorably to the 10 year weight loss of 14-25% seen after bariatric surgery.[76] Considering that bariatric surgery is an invasive and expensive procedure that can only treat a minority of the rapidly growing obese population, non-surgical interventions that mimic the metabolic benefits of bariatric surgery, with a reduced morbidity and mortality burden, are tenable alternatives.[77] To put this in context, the Look AHEAD Trial – which investigated the effects of an intensive lifestyle intervention – found a weight loss 6 % in the intervention group (in the control group the weight loss was 3.5%).[78] Obesity drugs (orlistat, lorcaserin, naltrexone-bupropion, phentermine-topiramate, and liraglutide) only results in a short-term (1 year) weight loss of around 5%.[79]
Conclusion
Accumulating evidence from long-term real-life studies of testosterone therapy in obese testosterone deficient men suggests that testosterone therapy merits serious consideration among healthcare professionals who are dealing with the rapidly growing number of men who are overweight/obesity and/or have the metabolic syndrome.
- 28 February 2017
- Written by Monica
Most men with testosterone deficiency need testosterone therapy for the rest of their life in order to achieve and maintain best possible health outcomes. Therefore, studies that investigate the effects of testosterone therapy in real-life are needed, to shed light on adherence and health outcomes in routine clinical practice.[1] While randomized controlled trials (RCTs) are gold standard in medical research [2, 3], RCTs are conducted in highly controlled environments and therefore their results may not carry over to the uncontrolled setting of real-life.[1] It is increasingly recognized that conclusions drawn from RCTs are not always a useful aid for decision-making because evaluating the value of a drug or technology requires an understanding of its impact on current clinical practice and management of patients in a real-life setting.[4]
A series of “real-life studies” have been conducted, all showing numerous health benefits of testosterone therapy in testosterone deficient (hypogonadal) men and confirming its safety, with an observation period of up to 17 years.[5-23] Here I summarize the results from the most recent real-life study, published February 9th 2017 in the Journal of Cardiovascular Pharmacology and Therapeutics which investigated the long-term effects and safety of testosterone therapy for up to 8 years in testosterone deficient men attending a urological office.[5] Differences in cardiovascular risk factors and deaths with testosterone therapy were compared to those seen in testosterone deficient men not receiving testosterone therapy but attending the same urological office.[5]
Key Points
- Long-term testosterone therapy for 8 years in obese men with testosterone deficiency reduces deaths and non-fatal heart attacks and strokes, compared to men not receiving testosterone therapy.
- The testosterone-group has an estimated reduction in deaths (mortality) between 66% and 92% compared to non-treated men.
- As expected, hemoglobin and hematocrit increased in the testosterone treated group, but levels remained within the physiological reference ranges.
- In the testosterone treated group, 7 patients (1.9%) were diagnosed with low-grade prostate cancer. In the untreated (control) group 12 patients (4.1%) were diagnosed with prostate cancer.
- This study confirmed the well documented improvements in lipid profile, especially reduction in non-HDL levels, and glycemic control (marked reduction in HbA1c from diabetic to normal glycemia).
- Being conducted in a real-life setting – as opposed to a controlled study environment – this study provides evidence that long-term testosterone therapy is both effective, safe and feasible in clinical practice, and importantly results in a reduction in "hard clinical endpoints".
What is known
Numerous studies have shown that testosterone therapy reduces waist circumference, body fat mass, blood pressure, blood glucose and HbA1c, increases lean body mass and insulin sensitivity, and improves lipid profiles.[9, 15, 24-30] Since obesity, dyslipidemia, insulin resistance, hyperglycemia, metabolic syndrome, hypertension and diabetes are well established cardiovascular risk factors, any therapeutic modality that ameliorates these components is expected to reduce cardiovascular risk. Despite this, a few flawed studies alleged that testosterone therapy would increase cardiovascular risk.[31-34] However, after having reviewed the available evidence on testosterone therapy and cardiovascular risk [35], the FDA denied the petition to place a black box warning about cardiovascular risk on testosterone products [36] and the European Medicines Agency (EMA) denied the allegations that testosterone therapy would increase cardiovascular risk.[37] Below are the results from a new long-term study which confirms the safety of testosterone therapy and actually shows reduced cardiovascular risk and mortality.[5]
What this study adds
Of 656 men (mean age: 61 years) with total testosterone levels 12.1 nmol/L (349 ng/dL) or lower and symptoms of hypogonadism, 360 received testosterone undecanoate injections 1000 mg every 12 weeks following an initial 6-week interval, for up to 10 years. This treatment group was compared to a control group made up of 296 men who had opted to not receive testosterone therapy. Measurements were taken at least twice a year and 8-year data were analyzed for the outcomes summarized in table 1.
Table 1: Effect of long-term (8 years) testosterone therapy on testosterone levels and metabolic outcomes.[5]
| Outcome | Testosterone treated group | Control group |
| Total testosterone levels | ↑ 283 to 476 ng/dL (9.8 to 16.5 nmol/L) | ↓ 277 to 260 ng/dL (9.6 to 9 nmol/L) |
| Anthropometric Parameters Body weight (lb) Waist circumference (in) BMI (kg/m2) | ↓ 229 to 192, -17.0% ↓42 to 38 ↓ 33 to 28 | ↑ 202 to 204, +1.5% ↑ 42 to 43 ↑ 29 to 30 |
| Glycemic control Fasting glucose HbA1c | ↓103 to 94 mg/dL ↓6.9% to 5.6% | No change ↑from 6.1% to 6.4% |
| Hemodynamics Systolic blood pressure (SBP) Diastolic blood pressure (DBP) Pulse pressure Rate pressure product | ↓151 mmHg to 130 mmHg ↓ 91 mmHg to 74 mmHg ↓61 mmHg to 56 mmHg ↓ 11 751 to 9421 | ↑ 139.5 mmHg to 140.3 mmHg ↑ 80 mmHg to 81 mmHg No change ↑ 10 623 to 10 890 |
| Lipid Profile (mg/dL) Total cholesterol LDL HDL Triglyceride TC/HDL ratio non-HDL | ↓ 278 to 186 ↓ 162 to 104 ↑ 54 to 73 ↓ 275 to 186 ↓ 5.6 to 2.6 ↓ 224to 113 | ↑ 244 to 263 ↑ 135 to 155 ↑ 50 to 62 ↑ 257 to 75 ↑ 6.2 to 5.6 (not significant) ↑ 194 to 201 |
| Liver Function Enzymes (U/L) AST ALT | ↓ 40 to 16 ↓ 42 to 16 | ↑ 23 to 40 ↑ 27 to 44 |
Safety Parameters
As expected, hemoglobin and hematocrit increased in the testosterone treated group, but levels remained within the physiological reference ranges.
In the testosterone treated group 7 patients (1.9%) were diagnosed with low-grade prostate cancer. In the untreated (control) group 12 patients (4.1%) were diagnosed with prostate cancer.
Death (mortality), nonfatal heart attack and stroke
There were 26 nonfatal heart attacks and 30 nonfatal strokes in the control group and none in the testosterone-treated group. There were 2 deaths in the testosterone-treated group, none was related to cardiovascular events. One was attributed to postsurgical thromboembolism and the other due to traffic accident. In the non-treated control group, there were 21 deaths, 19 of which were due to cardiovascular events (5 heart attacks, 4 stroke, 7 heart failure, 2 thromboembolism, 1 lung embolism).
The estimated reduction in mortality for the testosterone-group was between 66% and 92%. Figure 1 illustrates the differences in mortality, heart attack and stroke incidences between the groups.
Figure 1: Differences in mortality, heart attack and stroke between testosterone treated men and non-treated men.
Comments
This is the first long-term observational study that includes a comparison (control) group.[5] It confirms the safety and efficacy found in previous long-term real-life studies [5-23] and adds new important data. Several findings in this study deserve attention.
Liver function enzymes
The marked reduction in liver function enzymes in the testosterone treated group may suggest a potential reduction in liver fat content and inflammatory activity.[38, 39] It has previously been demonstrated that testosterone therapy reduces liver fat (accurately measured by CT imaging) in obese men.[40] There is a significant correlation between abdominal obesity and liver fat content (determined by liver biopsy during obesity surgery in severely obese men) [41] and numerous epidemiological studies shown that lower testosterone levels are associated with the development of NAFLD.[42] Considering that the prevalence of nonalcoholic fatty liver disease (NAFLD) is especially high in obese men [43], this merits further investigation.
Glycemic control
HbA1c is used to diagnose prediabetes and diabetes. The threshold for diabetes is HbA1c ≥ 6.5% and prediabetes is present when HbA1c is between 5.7% and 6.49%.[44, 45] As seen in table 1, testosterone treatment reduced glycemia from the diabetic range (HbA1c 6.9%) to normal range (HbA1c 5.6%). Going from diabetic glycemia to normal glycemia is a marked improvement, as most interventions only reduce glycemia from prediabetic to normal or diabetic to prediabetic. As expected, in the control group there was a worsening in glycemic control with an increase in HbA1c from 6.1% to 6.4%, to near diabetic glycemia (HbA1c 6.5%).
Pulse pressure
Pulse pressure (calculated as systolic blood pressure – diastolic blood pressure) is a marker of arterial stiffness [46-48] and is associated with greater risk of cardiovascular and all-cause mortality.[49] This study found a significant reduction in pulse-pressure in the testosterone treated group by 5 mmHg, while no change was seen in the control group. The importance of pulse pressure was highlighted in a study which found that a high pulse pressure in men is an independent predictor of cardiovascular mortality in both hypertensives and in those considered as having normal blood pressure, and it was suggested that this parameter can be useful when evaluating cardiovascular risk.[50]
Rate-pressure product
The rate-pressure product (RPP) (calculated as the product of heart rate and systolic blood pressure) is a reliable indicator of myocardial oxygen consumption and hemodynamic stress, and it is widely used clinically, especially in exercise interventions and rehabilitation.[51, 52] The rate pressure product (RPP) is associated with myocardial perfusion imaging (MPI) and it has been suggested that the cardiovascular risk with (pre)hypertension may be linked to the rate pressure product and BMI.[53] The study reported here found a significant reduction in RPP and significant increase in RPP in the testosterone and control groups, respectively.[5] This suggests that testosterone therapy may improve cardiac oxygen efficiency and reduce hemodynamic stress.
non-HDL cholesterol
This study is also notable for reporting a marked reduction in non-HDL cholesterol (non-HDL or non-HDL-C).[5] When triglyceride levels exceeds 150 mg/dL – as is commonly seen in patients with the metabolic syndrome, obesity, diabetes and cardiovascular disease - LDL particle number, apoB and VLDL levels increase without concomitant elevations in LDL-C.[54-56] Thus, non-HDL is more reflective of atherogenicity in people with elevated triglycerides.[57]
Several society guidelines for management of dyslipidemia for cardiovascular disease have recently added non-HDL as a primary treatment target. The International Atherosclerosis Society (IAS) Position Paper on the management of dyslipidemia considers non-HDL as an alternative to LDL-C as target of therapy, and actually favors adoption of non-HDL as the major target of lipid-lowering therapy.[57] The IAS expects that in future guidelines non-HDL will replace LDL-C as the best treatment target.
The European Society of Cardiology (ESC) / European Atherosclerosis Society (EAS) guideline states that non-HDL can provide a better risk estimation compared with LDL-C, in particular in patients with the metabolic syndrome or diabetes, who commonly have elevated triglyceride levels.[58]
Notably, the National Lipid Association (NLA) states that while non-HDL and LDL-C are co-primary treatment targets, non-HDL is the superior treatment target for modification.[59] Non-HDL levels and changes during treatment of dyslipidemia are more strongly associated with reduced risk for atherosclerotic coronary heart disease (CHD) than changes in LDL-C, or on-treatment levels of LDL-C.[59]
According to the 2017 AACE, ACE Dyslipidemia Clinical Practice Guidelines Update, the non-HDL treatment goal is 130 mg/dL for patients with two other risk factors, and 100 mg/dL for patients with two other risk factors plus diabetes or coronary, carotid or peripheral vascular disease.[60] In light of this, the marked reduction in non-HDL from 224 mg/dL to 113 mg/dL in testosterone treated men (and increase from 194 mg/dL to 201 mg/dL in non-treated men) should be highlighted.
Cardiovascular events and deaths
Regarding the debated issue of testosterone therapy and major cardiovascular events and mortality it is of particular interest is that there were only 2 deaths in the testosterone treated group, and none was related to cardiovascular events. Notably, in the non-treated control group there were 21 deaths, 19 of which were related to cardiovascular events. Furthermore, there were 26 nonfatal heart attacks and 30 nonfatal strokes in the control group but none in the T-treated group. In addition to all the beneficial changes in waist circumference reduction, weight loss and metabolic parameters that many studies have shown before, this is the first long-term study with a control (non-testosterone treated) group showing that this actually translates into reductions “hard clinical outcomes” in real-life.
The reduced incidence of heart attack, stroke, and death in testosterone treated hypogonadal men is in agreement with prior observational studies [12, 61-71] and two large meta-analyses of RCTs.[72, 73] The safety and cardiovascular protection of testosterone therapy was confirmed in the Testosterone Trials RCT, which found that during the follow-up year after the first year of testosterone therapy, there were 8 heart attacks in the placebo group compared to 1 in the testosterone group.[74] The longest duration RCT conducted at this point lasted for 3 years and also confirmed the safety of testosterone therapy.[75] An interesting finding in this study – which was not reported in the abstract - was that in men not taking statins, one marker of atherosclerosis (coronary artery calcium) was significantly lower in the testosterone group than in the placebo group.[75]
It is also notable that a another real-life study of men with testosterone deficiency and a history of cardiovascular disease, who received testosterone therapy for up to 8 years, no patient suffered a major adverse cardiovascular event during the full observation time.[12] In this study, cardio-metabolic parameters (lipid profile, glycemic control, blood pressure, heart rate, and pulse pressure), weight and waist circumference all improved significantly and sustainably [12], similarly to the results found in the study reported here.[5] Importantly, these improvements occurred even though patients were treated with statins, which suggests that statin treatment alone is inadequate. Thus, testosterone therapy may also be effective as an add-on treatment for secondary prevention of cardiovascular events in testosterone deficient men with a history of cardiovascular disease.[12]
Clinical practice relevance
Achievement of therapeutic testosterone levels - i.e. testosterone levels high enough (within the physiological range) – is essential for health benefits to occur.[66] The study reported here provides critical information on the long-term safety and effectiveness of testosterone therapy in clinical practice, as well as especially relevant data on adherence in the general population of men attending urological clinics.[5] It is notable that patients in the testosterone treated group achieved 100% medication adherence, as the testosterone injections were given in the doctor’s office and documented. This shows that injections of testosterone undecanoate at 12-week intervals is practically feasible in routine clinical practice, even in the long-term (the maximal observation duration was 10 years).[5]
The combined evidence base from both RCTs [72, 73] and observational studies [12, 61-70] is now strongly supportive of beneficial cardiovascular effects of testosterone therapy in hypogonadal men, which is accompanied by a reduction in cardiovascular mortality. In obese men, long-term testosterone therapy with testosterone undecanoate injections at 12 week intervals is clearly feasible in routine clinical practice and results in sustained weight loss and reductions in waist circumference and BMI without weight regain.[5-23] Interestingly, the 8 year weight loss of 17-24% with testosterone therapy [5] compares favorably to the 10 year weight loss of 14-25% seen after bariatric surgery.[76] Considering that bariatric surgery is an invasive and expensive procedure that can only treat a minority of the rapidly growing obese population, non-surgical interventions that mimic the metabolic benefits of bariatric surgery, with a reduced morbidity and mortality burden, are tenable alternatives.[77] To put this in context, the Look AHEAD Trial – which investigated the effects of an intensive lifestyle intervention – found a weight loss 6 % in the intervention group (in the control group the weight loss was 3.5%).[78] Obesity drugs (orlistat, lorcaserin, naltrexone-bupropion, phentermine-topiramate, and liraglutide) only results in a short-term (1 year) weight loss of around 5%.[79]
Conclusion
Accumulating evidence from long-term real-life studies of testosterone therapy in obese testosterone deficient men suggests that testosterone therapy merits serious consideration among healthcare professionals who are dealing with the rapidly growing number of men who are overweight/obesity and/or have the metabolic syndrome.



